Osteoporosis
Osteoporosis is a common medical condition. Unlike cold, cough, headache, raised blood pressure, we do not perceive osteoporosis but, in most instances, it reveals itself only with the complications, and that is a bone fracture. If we search for the causes of bone fracture in elderly patients and post-menopausal lady, we will see that osteoporosis is the main factor! In this post, we are going to learn osteoporosis in great details.
Let us know the definition of Osteoporosis
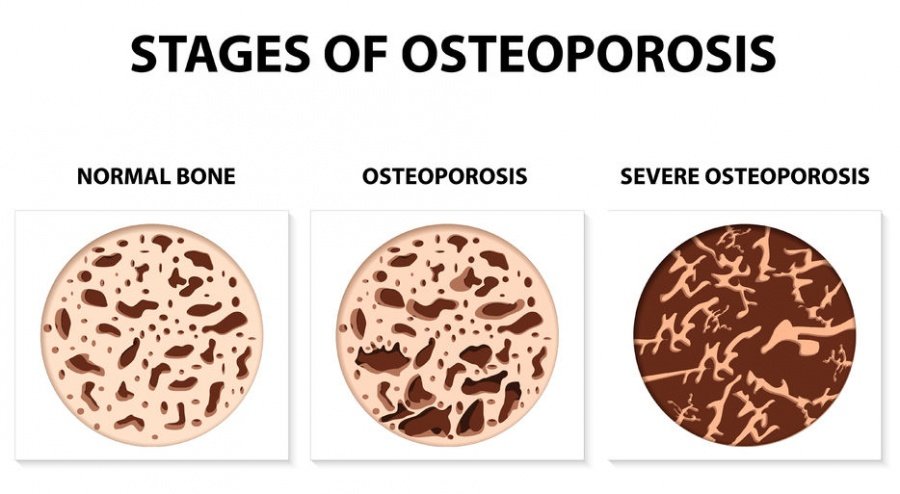
The meaning of the word osteoporosis is porous bone. When the density of a bone is reduced from its normal mass per unit volume, we call the condition osteoporosis. It can be defined differently as the increased fragility of bones. That means when a bone reduces mass per unit volume it becomes more fragile and the chances of fracture increases in many folds. Calcium is the main determinants of bone mass density. Hence, osteoporosis has a direct relationship between body and bone calcium levels. The diseases or conditions which alter the normal calcium levels, invite osteoporosis.
Normally, it is a disease of post-menopausal ladies and elderly men (some disease conditions may bring it earlier). One of female sex hormone, Estrogen, has a major role in maintaining normal calcium levels in bones. When a female reaches her menopause, and the support of estrogen is stopped, the body starts losing calcium at a much faster rate. Within the next 5-10 years, osteoporosis develops and weight-bearing bones affects mostly. Sixty-five years onwards, the fracture rate is 3-5 times higher than before.
Hormone Replacement Therapy (HRT) for post-menopausal ladies has prevented estrogen deficiency, and thus osteoporosis. But the development of breast cancer associated with HRT has brought a negative impact on it.
Osteoporosis is common but silent, measurable its extent, preventable but potentially lethal. A patient with osteoporosis, even with minor trauma, fracture might happen. Osteoporosis usually presents with a fracture and it is the first manifestation of underlying osteoporosis. The most affected (e,g, fracture) bones are the lower end of the forearm (named Colles fracture), the neck of the femur (bones of the thigh) and vertebra (backbone). Vertebral collapse (height shrinkage) is the hallmark of osteoporosis.
What are the risk factors/ causes of developing osteoporosis? (Apart from menopause)
Broadly, we can divide the factors/causes into 3 categories:
Constitutional/ non-modifiable risk factor (we can’t do anything about these):
- Sex: Female sex is more prone to osteoporosis (due to menopause)
- Ageing
- Body build: A thin person with short stature and BMI less than 18 is more susceptible
- Race: Asian and Caucasians are mostly affected
- Family history: If there is a history of hip fracture in ladies of a family before the age of 75 years, the future generations are at higher risk
- Late menarche, early menopause and long-standing secondary amenorrhea in between, all these 3 conditions lead to reduced estrogen hormone in a female.
Modifiable risk factors:
- Cigarette smoking and high alcohol intakes are both considered as risk factors for developing osteoporosis. Smoking a cigarette brings not a single benefit while taking a small amount of alcohol may be beneficial for some condition. But an excess of it brings bad outcome.
- Lack of vitamin D and low calcium intake are the main risk factors for osteoporosis. If these food trends persist for a long time, fragile bones will be the end result.
- Physical inactivity is also associated with an increased risk of osteoporosis
Medical causes of osteoporosis:
- Anorexia nervosa; an eating disorder where the patients can’t even eat the minimum amount of food required for maintaining a healthy body.
- Malabsorption syndrome: A collection of disorders of the digestive system where the patient eats but the ingredients of food don’t go into the bloodstream; hence the body doesn’t get what is necessary. Coeliac disease is at the top of the list of the disorders.
- Prolonged immobilization (in disabled patients due to stroke, or during the recovery period after major surgery)
Some hormonal disorders that may lead to osteoporosis:
- Cushing syndrome: An excess of cortisol in our blood
- Diabetes mellitus
- Hyperparathyroidism
- Thyrotoxicosis (an excess of thyroid hormone)
- Hypogonadism/sex hormone deficiency
- Acromegaly (an excess of Growth hormone)
Some drugs are responsible for osteoporosis:
- Corticosteroids
- Anti-epileptic drugs, especially hepatic enzyme Inducers (Carbamazepine, phenytoin, phenobarbital and primidone)
- Thiazolidinediones for diabetes mellitus
- Long-term use of heparin
- Excessive use of thyroid hormone which turns into drug-induced thyrotoxicosis
- Prostate and breath cancer hormone therapy
Treatment options for osteoporosis
The number one priority is to prevent osteoporosis. And number two is to reduce further loss of bones. That means our main concern must be on preventing developing of osteoporosis and unfortunately, if already developed, then to reduce further loss. The ways of reversing the process of osteoporosis and regaining the lost bones are yet to come. No treatment is available which can replace the lost bones effectively. Some agents have shown effectiveness in preventing further losses of bones but their side effects are also problematic.
Following treatment options are available which help the patient preventing further loss of bone, and hence preventing fractures. The important side effects are mentioned too.
- HRT (Hormone replacement therapy): Long-term use may cause breast cancer.
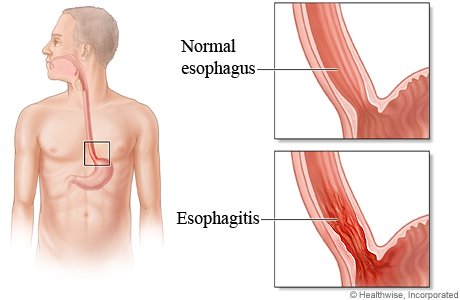
- Bisphosphonates: Oesophagitis and osteonecrosis of the jaw are two important side effects. (Alendronate, etidronate, risedronate, zoledronic acid, etc are included in this group).
- Raloxifene: Some reports of vascular complications.
- Teriparatide: It has the potentiality in increasing bone formation.
- Denosumab: Osteonecrosis of Jaw is the side effect.

What preventive measures should be taken?
Adequate intake of Calcium, either through diet or oral supplementation: Recommended daily dose of calcium is 1200-1300 mg for both sex. Postmenopausal lady and those whose dietary intake is not adequate (due to any reason), should take oral supplementation of calcium. Usually, two forms of oral calcium tablets are available; calcium carbonate and calcium citrate. Anyone of them can be taken but later one is absorbed better in the digestive tract.
Sunlight exposure and Vitamin D supplementation: Significant exposure to sunlight of the face, arms and hands are necessary to produce enough vitamin D in our body. As per rule, at least 15-30 minutes exposure (in all climate but in winter it might need up to 50 minutes per day) is required for getting sufficient natural vitamin D. People at risk should measure their blood vitamin D level (25-hydroxy vitamin D) and if the count is below the optimal level (at least 75 nmol/L), oral supplementary Vitamin D should be taken. In that case, daily 25-50 mcg or 1000-2000 IU of vitamin D in the form of cholecalciferol have to be taken orally.
Regular exercise: Moderate exercise against gravity, such as walking (a brisk walk of 30 times at least 5 times per week), running, jogging etc. are better to do on a regular basis.
Lifestyle moderation: Smoking cessation is highly recommended. Limiting alcohol and caffeine intake are highly appreciated. Improvement of the nutritional status (if not optimum) and maintaining the BMI over 18. Taking extra care to prevent fall is necessary (avoid sedative medications).
Use of hip protectors: Osteoporotic patients may wear hip protectors

Picture of a hip protector (image source)



0 Comments